Bloodborne Pathogens and Needlestick Prevention
Hazard Recognition
The CDC estimates that there are approximately 18 million workers in the health care industry many of whom are at risk for occupational exposure to bloodborne pathogens. These bloodborne pathogens include human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV). Other organisms that can be transmitted through blood or other potentially infectious materials (OPIM) include cytomegalovirus (CMV), Epstein-Barr virus (EBV), zika virus, and human parvovirus B19. Less commonly encountered bloodborne pathogens are, syphilis, babesiosis, brucellosis, other mosquito-transmitted diseases, and agents that can cause viral hemorrhagic fever such as the Marburg and Ebola viruses. The following references aid in recognizing workplace hazards associated with bloodborne pathogens.
- Healthcare Workers. National Institute for Occupational Safety and Health (NIOSH). 2024.
- Bloodborne Infectious Disease Risk Factors. National Institute for Occupational Safety and Health (NIOSH) Workplace Safety and Health Topic (2024).
- Bloodborne Pathogens - OSHA's Bloodborne Pathogens Standard. OSHA Fact Sheet (2011).
- Zika Virus. CDC.
- Cytomegalovirus (CMV) and Congenital CMV Infection. CDC.
- Cytomegalovirus - Overview. Occupational Safety and Health Administration.
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Centers for Disease Control and Prevention (CDC) (2024).
All occupational exposure to blood or other potentially infectious materials (OPIM) places workers at risk for infection from bloodborne pathogens. OSHA defines blood to mean human blood, human blood components, and products made from human blood. Other potentially infectious materials (OPIM) means: (1) The following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids; (2) Any unfixed tissue or organ (other than intact skin) from a human (living or dead); and (3) HIV-containing cell or tissue cultures, organ cultures, and HIV- or HBV-containing culture medium or other solutions; and blood, organs, or other tissues from experimental animals infected with HIV or HBV. See Worker protections against occupational exposure to infectious diseases for a comparison of OPIM covered by OSHA's Bloodborne Pathogens standard to other body fluids covered by standard and transmission-based precautions in healthcare.
Bloodborne Pathogens: Prevention, Immunization, Prophylaxis and Treatment
- Using Standard Precautions can reduce the chances of acquiring HBV, HCV, and HIV infections as well as infections from other bloodborne pathogens. Standard Precautions, introduced in 1996, expands on Universal precautions as it adds additional infection prevention elements.
- Comparison of Universal Precautions, Standard Precautions, and Transmission-based Precautions.
- HIV and Occupational Exposure | HIV in the Workplace | HIV/AIDS. CDC (2019).
- Occupationally Acquired HIV Infection Among Health Care Workers — United States, 1985–2013 - PMC. Centers for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report (MMWR) 63(53):1245-1246, (Jan 9, 2015).
- Prevention of HIV/AIDS: Post-Exposure Prophylaxis (including Healthcare Workers) - PMC. Infect Dis Clin North Am. 2013 Dec; 28(4):601-613.
- Immunization is available to protect individuals from acquiring hepatitis B virus (HBV). Treatment is also available for HBV infection, as is post-exposure prophylaxis to potentially prevent HBV infection if administered timely.
- Testing and clinical guideline management is available if there is a potential exposure to Hepatitis C Virus (HCV). There is CDC guidance that includes recommendations for a testing algorithm and Clinical Management for HCP with potential occupational exposure to hepatitis C virus.
- Testing and Clinical Management of Health Care Personnel Potentially Exposed to Hepatitis C Virus — CDC Guidance, United States, 2020 | MMWR. Centers for Disease Control and Prevention (CDC), Morbidity and Mortality Weekly Report (MMWR) 69(6);1-8, (July 2020).
- Guidelines for Health Care Personnel Exposed to Hepatitis C Virus. Centers for Disease Control and Prevention (CDC), Hepatitis C. Explore Topics. April 24, 2024
- Post-Exposure Prophylaxis is available to potentially prevent HIV if administered timely.
- Updated U.S. Public Health Service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. (September 25, 2013; Updated May 23, 2018).
- Interim Statement Regarding Potential Fetal Harm from Exposure to Dolutegravir – Implications for HIV Post-Exposure Prophylaxis (PEP). (2018).
- Guidelines for Clinical Care for persons living with HBV, HCV, and / or HIV. Management of healthcare personnel living with hepatitis B, hepatitis C, or human immunodeficiency virus in US healthcare institutions. Infect Control Hosp Epidemiol. 2022 Feb;43(2):147-155.
- Strategies for preventing Zika Virus Infection. Protecting Workers from Zika. Centers for Disease Control and Prevention (CDC) (May 15, 2024).
Bloodborne Pathogens: Healthcare Settings

The major source of bloodborne infections in healthcare settings is via percutaneous injuries from needles or other sharps. Mucosal exposure also occurs but is less common.
- OSHA Bloodborne Pathogen Standard.
- Hospitals. OSHA eTool. Focuses on some of the hazards and controls found in the hospital setting and describes standard requirements as well as recommended safe work practices for employee safety and health (2021-2022).
- Healthcare-associated Infections (HAI). Centers for Disease Control and Prevention (CDC) (2021).
- EPINet. The University of Virginia, International Healthcare Worker Safety Center. Since 1992, the Exposure Prevention Information Network (EPINet) system has continuously provided standardized methods for recording and tracking percutaneous injuries and blood and body fluid contacts. EPINet consists of a Needlestick and Sharp Injury Report, a Blood and Body Fluid Exposure Report, and software for entering, accessing, and analyzing the data from the forms (2018-2019).
- Healthcare. OSHA Safety and Health Topics. Healthcare. (2021).
- Dentistry. OSHA Safety and Health Topics. Dentistry.
- Medical and First Aid. OSHA Safety and Health Topics. First Aid Kit.
- Nursing Homes and Personal Care Facilities. OSHA Safety and Health Topics. Nursing Homes and Personal Care Facilities.
- NIOSH Hazard Review: Occupational Hazards in Home Healthcare. NIOSH CDC (2010).
- Applicability of Bloodborne Pathogens Standard to emergency responders, decontamination, housekeeping, and good Samaritan acts. Occupational Safety and Health Administration. (1992).
Bloodborne Pathogens: Non-Healthcare Settings
Although most BBP exposures occur in healthcare settings, other occupational groups are at risk. These include home health aides, personal care aides, childcare workers, and personal care and service workers. According to the 2021 US Census Bureau there are 109,545,164 of these workers. Law enforcement officers (LEO) and firefighters are also at risk. In 2022, the National Fire Protection Association (NFPA) estimated that there were more than 800,000 sworn LEOs and1,041,200 firefighters. Additionally, while the BBP directive states that the BBP standard does not cover construction, the standard does apply to employees, such as plumbers, performing maintenance activities which involve making or keeping a structure, fixture, or foundation in proper condition in a routine, scheduled, or anticipated fashion and who have reasonably anticipated exposure to blood or other potentially infectious materials while performing their jobs. The standard also covers staff supporting intravenous drug users.
- Janitorial employees' exposure to bloodborne pathogens. Occupational Safety and Health Administration (1992).
- The hotel/motel industry and the bloodborne pathogens standard. Occupational Safety and Health Administration (1993).
- Bloodborne pathogens standard and the construction industry. Occupational Safety and Health Administration (1993).
- Blood-borne pathogens among firefighters and emergency medical technicians - PubMed (2005).
- First Responders: Protect Your Employees with an Exposure Control Plan. NIOSH CDC (2008)
- First Responders: Informational Poster on Bloodborne Pathogen Exposures. NIOSH CDC (2014).
- Bloodborne Pathogen Exposure. NIOSH CDC (2014).
- HHE Report No. HETA-2016-0121-3284, Evaluation of Needlestick Injuries and Other Exposures to Bloodborne Pathogens Among Officers in a City Police Department. CDC (2016).
- Federal Law Enforcement Officers, 2020 – Statistical Tables. Bureau of Justice Statistics (2020).
- Law Enforcement Facts - National Law Enforcement Officers Memorial Fund. (2021).
- Addressing the Opioid Overdose Epidemic in Construction: Minimize Work Factors that Cause Injury and Pain. CDC (2021).
- National Family Caregivers Month: November 2022. United States Census Bureau.
- Protecting Law Enforcement Officers from Sharps Injuries. NIOSH CDC (2022).
- Coverage of Childcare Workers under Scope of Occupational Exposure to Bloodborne Pathogens. Occupational Safety and Health Administration.
- Employees (daycare workers) required to provide First Aid are covered by 1910.1030. Occupational Safety and Health Administration.
- CFOC Standards Database | National Resource Center. Caring for our Children. Prevention of Exposure to Blood and Body Fluids (2024).
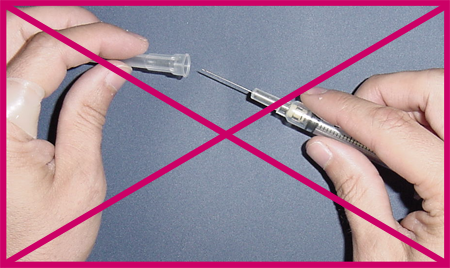
Needlesticks
- Potential for Occupational Exposure to Bloodborne Pathogens from Cleaning Needles Used in Allergy Testing Procedures. OSHA Health Information Bulletin (HIB), (September 21, 1995).
- What Every Worker Should Know: How to Protect Yourself From Needlestick Injuries. U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Publication No. 2000-135, (July 1997). Discusses pathogens that pose the most serious health risks.
- Selecting, Evaluating, and Using Sharps Disposal Containers. U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Publication No. 97-111, (January 1998). This publication presents a comprehensive framework for selecting sharps disposal containers and evaluating their efficacy as part of an overall needlestick injury prevention plan. It reviews the Occupational Safety and Health Administration (OSHA) bloodborne pathogens standard and recommends containers based on a site-specific hazard analysis. It establishes criteria and provides tools for evaluating the performance of sharps disposal containers.
- Preventing Needlestick Injuries in Health Care Settings. U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Publication No. 2000-108, (November 1999). NIOSH warns that health care workers who use or may be exposed to needles are at increased risk of needlestick injury.
- Disposal of Contaminated Needles and Blood Tube Holders Used for Phlebotomy. OSHA Safety and Health Information Bulletin (SHIB), (October 15, 2003). OSHA has concluded that the best practice for prevention of needlestick injuries following phlebotomy procedures is the use of a sharp with engineered sharps injury protection (SESIP), (e.g., safety needle), attached to the blood tube holder and the immediate disposal of the entire unit after each patient's blood is drawn.
- Medical & Dental Offices: A Guide to Compliance with OSHA Standards. OSHA Publication 3187, (2004). Provides a glimpse of the most frequently found hazards in medical and dental offices.
- Bloodborne Pathogens - Protecting Yourself When Handling Contaminated Sharps. OSHA Fact Sheet, (January 2011).
- Home Healthcare Workers: How to Prevent Needlestick and Sharps Injuries. U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Publication No. 2012-123, (February 2012).
- Safer needles rollout study identifies factors for implementation success. At Work, Issue 75, Winter 2014: Institute for Work & Health, Toronto, Canada. Good communication, gradual transition and outside support pave the way for new technology.
- Preventing Needlesticks and Sharps Injuries: Reflecting on the 20th Anniversary of the Needlestick Safety and Prevention Act. CDC (2020).
- Securing Medical Catheters. OSHA Fact Sheet.

